The white layer on eye can be a sign of a variety of eye conditions, ranging from benign growths to more serious disorders, like infections, inherited or developmental problems, and even cancers. This article explains the most common causes of white spots on the eye, along with their symptoms and possible treatment options. To keep your eyes healthy and your vision clear, it’s important to know when to seek urgent help from your doctor. Read on to get an understanding of the commonest causes of white spots on the eye.
Commonest Causes Of White Spots On The Eye
Following is a list of the five commonest causes of white spots on the eye. The symptoms, causes and treatments for each are are given in separate sections below
- Corneal Ulcer
- Pinguecula
- Cataract
- Cancer Of The Eye Surface (Squamous Cell Carcinoma)
- Leukocoria (White Reflex)
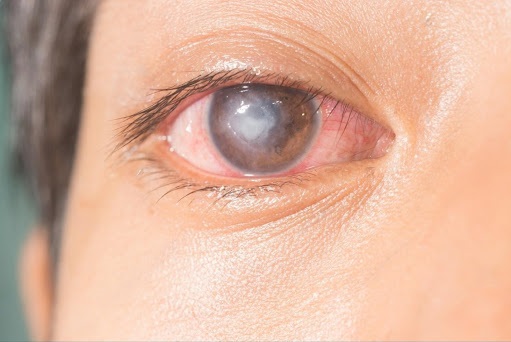
CORNEAL ULCER
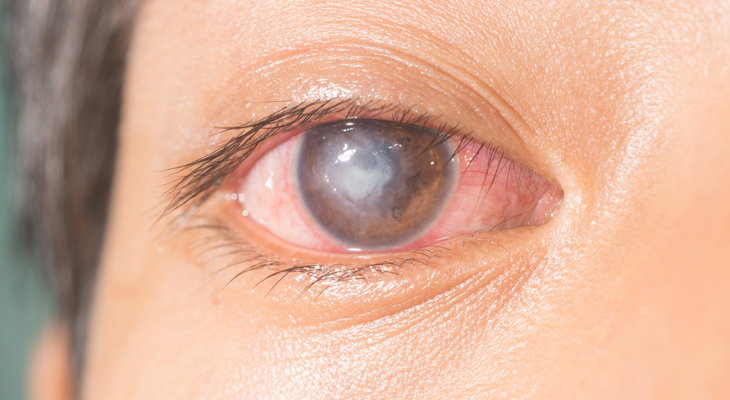
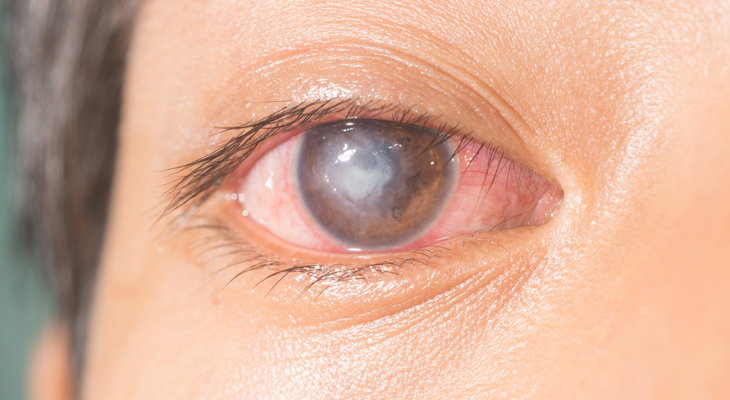
A corneal ulcer, is an open sore on the surface of the cornea, which is the clear front part of the eye. It occurs when the outer layer of the cornea becomes damaged, allowing micro-organisms to enter the cornea and cause an infectious sore that appears as a white spot. Sometimes corneal ulcers may occur due to collection of white blood cells in the cornea (without any microorganisms) that can release chemicals that cause an open sore.
Symptoms
-
- Severe eye pain
- White spot on the clear part of the eye (cornea)
- Redness (of the white of the eye)
- Blurry vision
- Light sensitivity
- Excessive tearing and/or sticky discharge
- Sensation of a foreign object in the eye
- Swelling of the eyelids
Note: if you have preexisting eye conditions that cause reduced sensations in the eye, or if your ulcer is from viruses, you may have very mild to no pain with corneal ulcers. Corneal ulcers are sight threatening infections of the eye, which is why early diagnosis and treatment is essential.
Causes
- Injury:
Trauma to the cornea can lead to a break in the protective barrier of cells that normally covers its surface. This can create an opening for micro-organisms (bacteria, fungi or viruses) to enter the cornea and lead to the formation of an infective sore (ulcer). The trauma may be from anything from a fingernail, to a sharp object hitting the eye.
- Improper contact lens use:
Improper use of contact lenses, which includes improper handling and storage, wearing lenses while sleeping, or swimming while wearing contact lenses can cause infective corneal ulcers. Contact lens wear causes micro trauma to the surface of the eye and reduced oxygenation of the surface cells. These factors make the eye surface more likely to get infected by micro-organisms especially when exposed to bugs present on unwashed hands, in stale lens solutions and in swimming pools.
- Certain Eye Diseases:
Dry eyes and eye allergies can change the normal surface conditions of the eye, leading to poor health of the surface of the eye, making it less resistant to infections. Both conditions also make the eyes irritated and itchy, leading to eye rubbing. Eye rubbing causes trauma to the eye surface and allows transfer of organisms from the eyelashes, eyelid skin and hands to the surface of the eye. All these factors combined make the eye surface more likely to develop ulcers.Other eye conditions such including those that reduce the sensations of the eye, those that cause misdirections of lashes towards the eyes, and disorders that prevent complete eye closure can also cause ulcers.
- Systemic diseases:
Immune system related disorders such as Rheumatoid Arthritis, Lupus and Wegener’s granulomatosis can lead to collection of white blood cells on the eye surface. These cells are abnormally activated and release chemicals that cause formation of an ulcer or sore on the surface of the eye.
- Poor immunity:
Poor immunity from conditions such as poor general health, cancer chemotherapy and HIV infection reduces the ability of the body to fight off infections and can result in infective ulcers.
Treatment
Treatment of corneal ulcers depends on the cause. It may include the following:
-
- Eye drops to treat the infection (antibiotics, anti-fungals and/or antivirals)
- Eye drops for pain relief
- Oral pain killers
- Oral anti-infectives (antibiotics, anti-fungals and/or antivirals)
- Steroid eye drops for immune related ulcers and in infective ulcers (only after the infection has been brought under control)
Final Outcome
If the ulcer is not timely treated it can lead to spread of infection with spread of infection into the inner parts of the eye. This is a very serious complication of corneal ulcers, as infection inside the eye may result in permanent loss of vision.
With treatment the ulcer usually heals, but leaves a white scar. The appearance of the scar may slightly improve over time. If the ulcer and resultant scar are in the central part of your cornea, they can cause decrease in vision that is not correctable with glasses or contact lenses. A corneal transplant may be needed to improve vision after central corneal scarring.
PINGUECULA
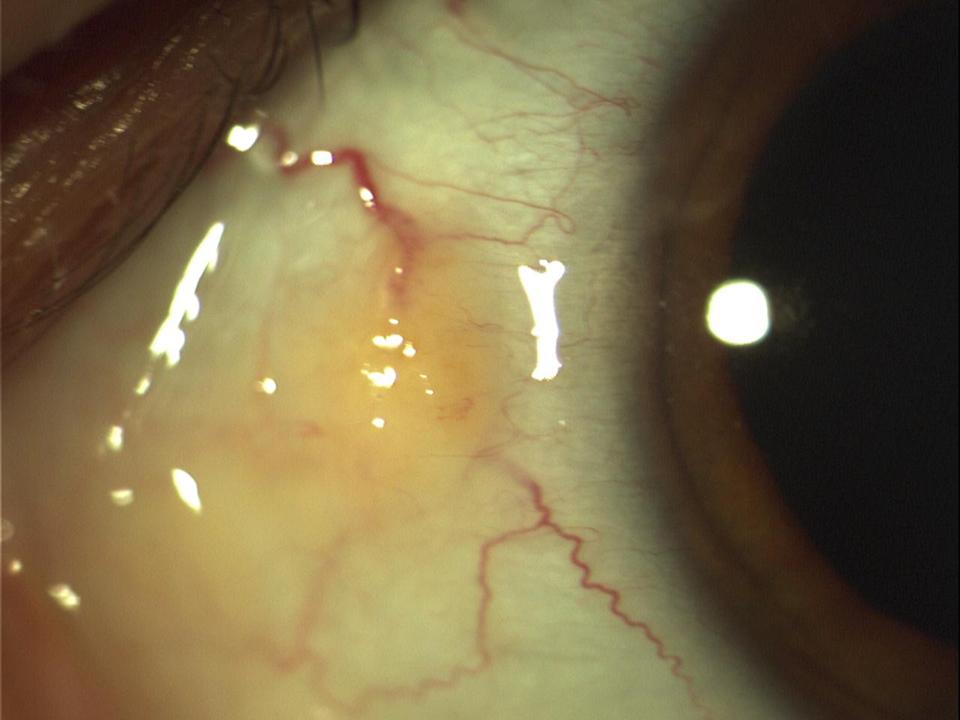
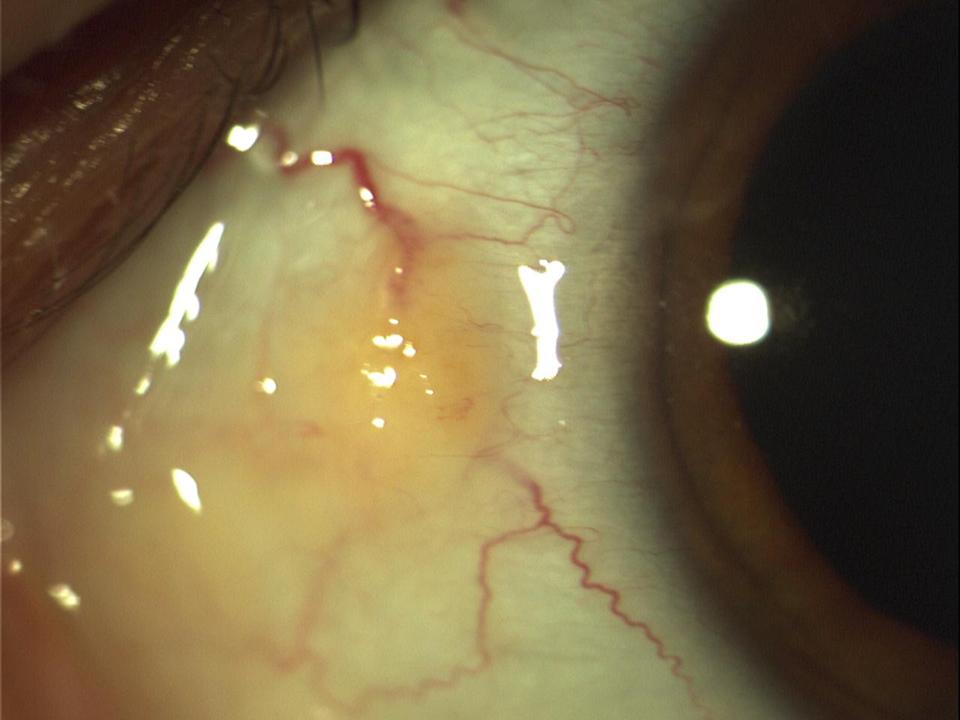
This is a harmless yellowish growth that occurs on the white of your eye, more commonly on the side of the eye that is closer to the nose. Often the growth is unnoticeable and present for quite some time but only detected when the eye becomes red from any cause. This is because this growth lacks blood vessels and when the eye is red, the yellow-white lesion stands out in comparison to the surrounding redness in the eye. Sometimes, the pinguecula itself may become inflamed (a condition called pingueculitis) resulting in a similar appearance of white on red.
Symptoms
-
- Often without any symptoms
- Yellow/white spot on the white of the eye
- If inflamed, may cause redness, foreign body sensation, irritation.
Causes
Pinguecula form from prolonged exposure to ultraviolet (UV) radiation, heat and wind – conditions that dry and degrade the surface of the eye.
Treatment
-
- Observation if not symptomatic
- Lubricant eye drops to soothe the eye, if irritated
- UV protection (sunglasses) and protection from dry dusty environments (protective goggles)
- Steroid drops for inflammation and irritation not resolving with the above measures
- If the appearance of the spot is displeasing, it can be excised as it does not disappear with the use of eye drops
Cataract
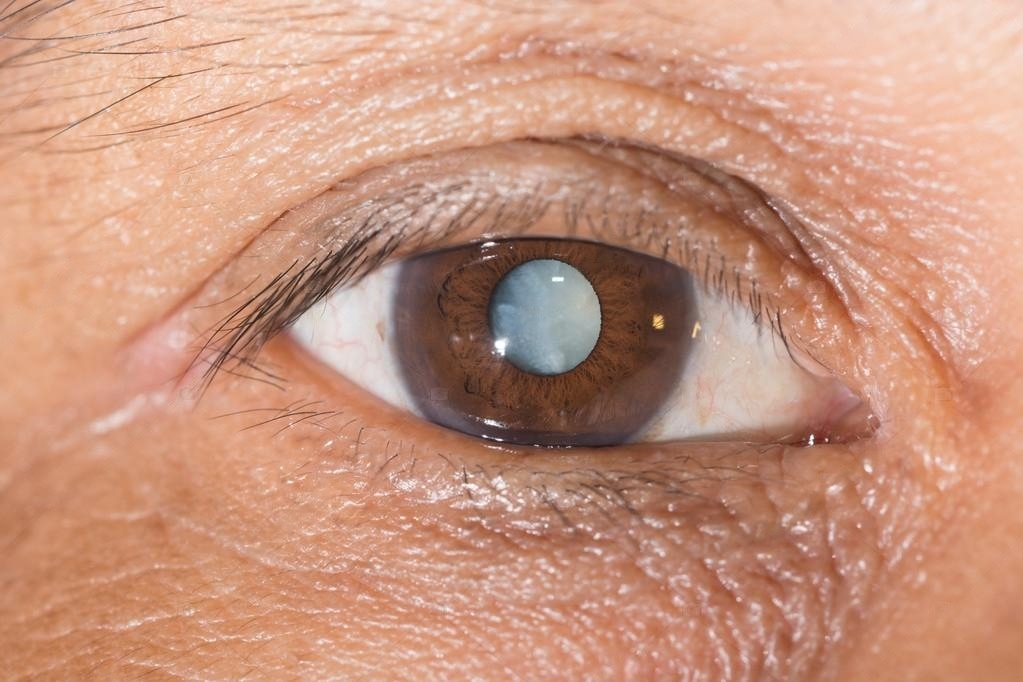
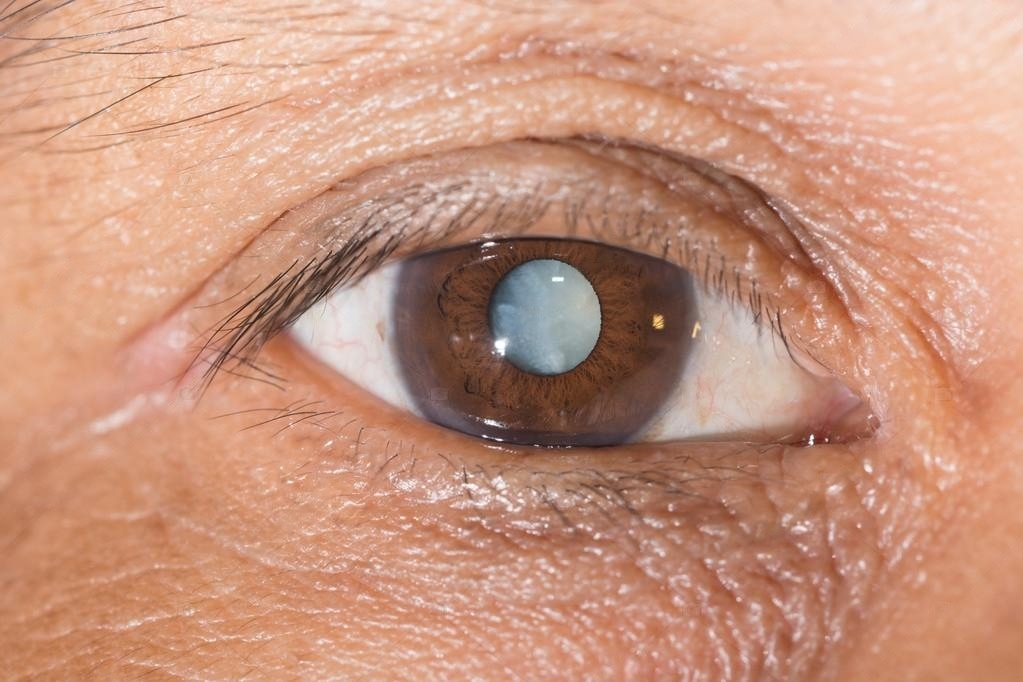
A cataract is a common eye condition resulting from clouding of the lens of the eye. The lens is a transparent structure located behind the iris (colored part of the eye). It plays a major role in focusing light at the back of the eye, allowing us to see clearly.
Symptoms
-
- Blurring of vision
- Difficulty seeing in bright or dim lighting
- Double vision
- Glare
Causes
Cataracts can result from a variety of causes including:
-
- Aging: These cataracts occur due to age related changes in the lens and are affected by a variety of inherited and environmental factors.
- Diabetes: Development of cataracts occurs at an earlier age and worsens faster in diabetics.
- High myopia: Individuals with high myopia often develop cataracts at an earlier age
- Congenital : These cataracts are disorders in development of the lens in the womb and are present since birth or develop soon after birth
- Injury: Injury to the eye, from either blunt or sharp objects can cause cataracts. Injury to the eye from chemicals, electric shock or radiation can also cause cataracts
- Medications: Most common medications associated with formation of cataracts are steroids and chlorpromazine
- Inflammation in the eye: Any disorder that causes inflammation in the eye can result in the development of cataracts
- Systemic disorders: Cataracts can result from a variety of systemic disorders like myotonic dystrophy, neurofibromatosis, atopic dermatitis
- Inherited eye conditions: Inherited eye conditions such as retinitis pigmentosa and stickler syndrome are associated with early development of cataracts
Treatment
Surgery is the only treatment for cataracts. Fortunately, most cataracts can be removed by a procedure called ‘phacoemulsification’ which a quick, safe and effective surgery that lasts around 20 minutes and gives excellent visual results.
CANCERS OF THE SURFACE OF THE EYE (Squamous Cell Carcinoma)
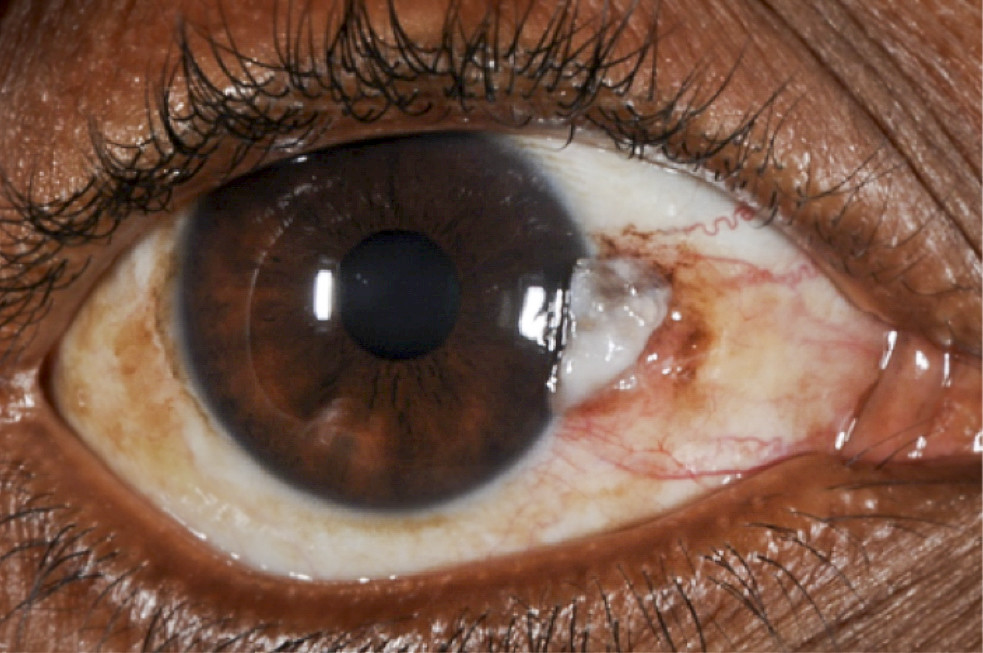
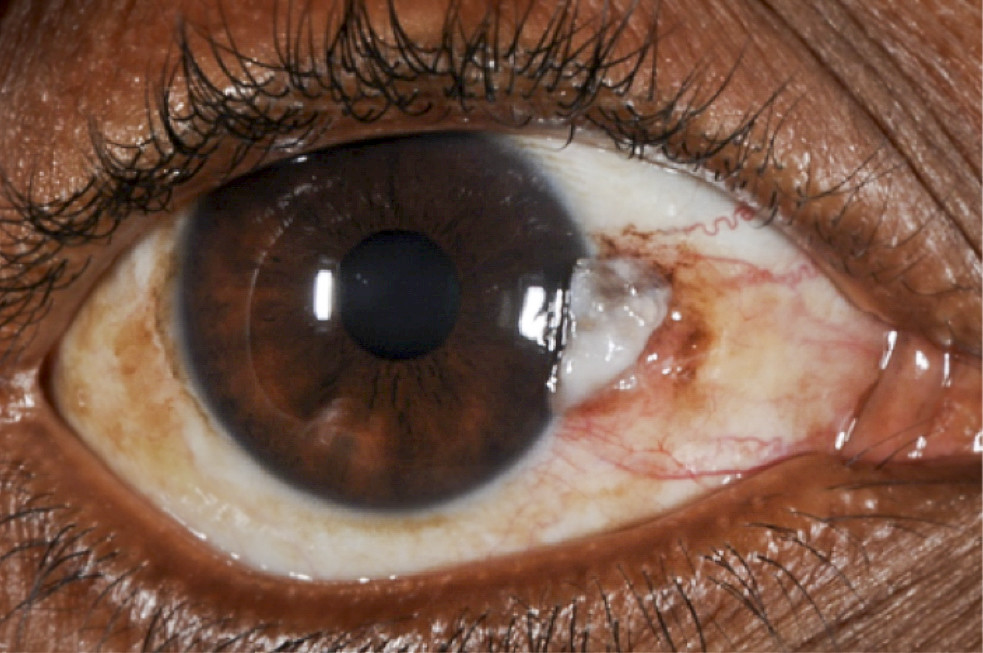
A squamous cell carcinoma (cancer of the surface cells) may appear as white or red lesion on the surface of the eye. It usually appears on the white of the eye (sclera) but may grow onto the clear part of the eye (cornea).
Symptoms
-
- Red-white growth (usually on the white of the eye)
- Usually painless (but with mild irritation)
- Increase in size over time
- Redness
- Irritation
Causes
-
- Increasing age
- Excessive sunlight (UV) exposure
- Pale complexion
- Smoking
- Exposure to certain chemicals like petroleum
- HIV infection
- Infection with human papilloma virus
Treatment
- Surgical removal of the growth along with added treatments like:
- freeze therapy (cryotherapy)
- anti-cancer (chemotherapy) injections into the lesion e.g. Mitomycin-C, 5-FFU, interferon alpha 2b
- Anti-cancer eye drops may also be prescribed after the surgery, to be used for weeks (Mitomycin-C, 5-FFU, interferon alpha 2b).
WHITE EYE REFLEX (Leucocoria)


Some disorders of the inside of the eye including eye cancers produce a white light reflex in the pupil (the central normally black portion of the eye). This white reflex is called leukocoria and is most commonly noticed in photos or when light falls into the eye at a certain angle. Most disorders causing leukocoria occur in childhood.
Symptoms
-
- Decrease in vision will be present with all of the above disorders
- Pain may or may not be present depending on the disorder and stage of disease
Note: the presence or absence of pain cannot help differentiate between cancerous and non-cancerous causes
Causes
Some of the commoner causes include:
-
- Retinoblastoma
- Coats disease
- Retinopathy of prematurity (ROP)
- Persistent fetal vasculature (PFV)
- Ocular toxocariasis and toxoplasmosis
- Familial exudative vitreoretinopathy (FEVR)
- Retinochoroidal coloboma
- Pediatric uveitis
- Retinal detachment
The above causes include infections, inherited disorders, disorders of development and cancers. Your eye doctor can differentiate between the above based on questioning, examination and further testing. It is extremely important to get your child evaluated by your eye doctor as soon as possible if a white reflex thought to be present.
Treatment
-
- The treatment of inherited and developmental disorders depends on the type of disorder and its severity. It may include lasers, freeze therapy, injection of medication into the eye and/or surgery.
- For cancers (e.g. retinoblastoma), treatment depends on the stage or severity of the tumor. Surgery, radiotherapy, chemotherapy and/or removal of the eye may be needed to prevent or limit spread.
- Infections of the eye may be treated with injection of medication into the eye, and oral anti infectives.
- The final outcome for vision depends on the type of disorder and its severity.
Conclusion
In conclusion, white spots on the eye can signal various eye issues, from harmless growths to more serious conditions like infections and even cancers. It’s important to pay attention to symptoms like pain, redness, and changes in vision and seek timely medical help when needed. Children with reduced vision and white spots on the eye should be examined by an eye doctor as soon as possible. Understanding the causes and symptoms of white spots on the eye can help guide you when to seek urgent help. Remember, early diagnosis and treatment are essential for maintaining good vision and eye health.