After undergoing cataract surgery, your vision may have cleared up, but you notice that it gradually began to cloud over again. After having an eye examination, you were diagnosed with PCO, or Posterior Capsular Opacification. You were also informed that in order to improve your vision, a laser procedure, known as a YAG capsulotomy would be required.
What is PCO precisely, and why did it occur? Was it something that could have been prevented? Will it result in issues with your eyes? What kind of treatments are possible?
This post will address not just the aforementioned queries but also all others related to Posterior Capsular Opacification and YAG capsulotomy.
What Is Posterior Capsular Opacification (PCO)?
PCO is a very common condition experienced by 1 in every 4 persons who have had cataract surgery.
It is the most common late side effect of cataract surgery.
Fortunately, a straightforward treatment can effectively correct this benign condition.
To understand what PCO is and how it impacts vision, it is necessary to have a basic understanding of cataract surgery.
Why Cataract Surgery Is Performed?
In order for us to view an object, light must pass through our eye, and be focused at the back of our eye. For light to reach the back of our eye, it must pass through various structures of the eye. These structures are transparent and in addition to letting light pass through them, they help focus it at the back of the eye.
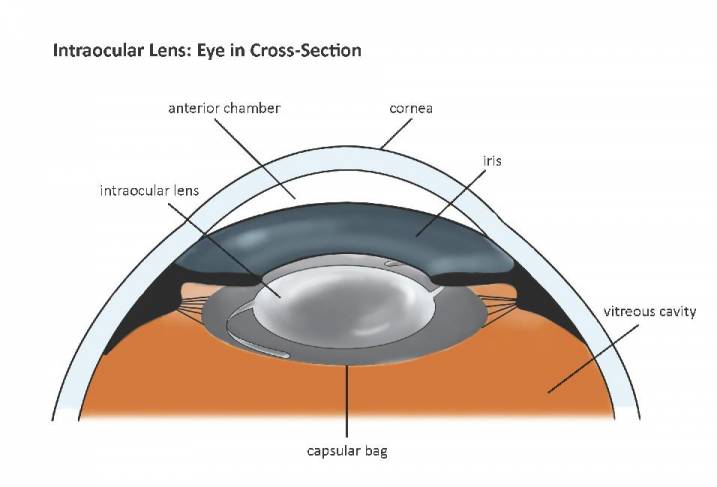
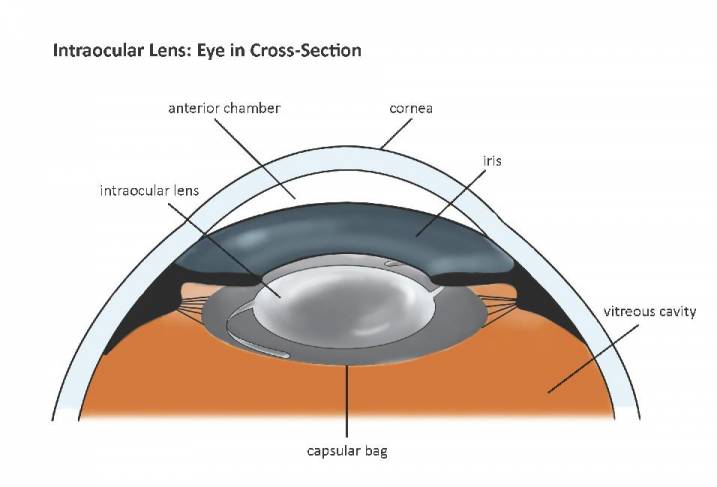
One of these structures is the lens of the eye, that is present behind the colored part of the eye (the iris). The lens is present inside a bag like structure and is suspended behind the iris by thread like attachments called the suspensory ligaments or zonules.
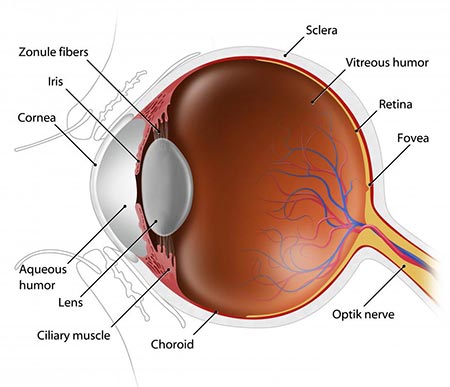
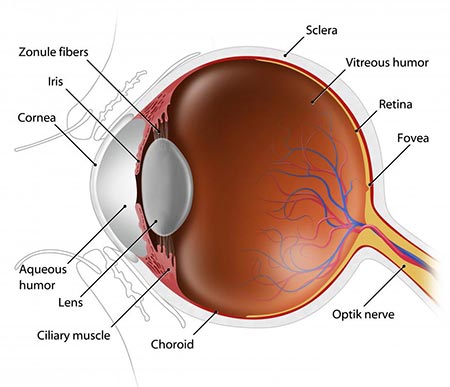
Normally the lens is transparent, allowing light to easily pass through it. Various factors, including aging, cause the lens to become cloudy and loose its transparency. This cloudy lens is called a cataract. Cataracts block light from reaching the back of the eye and cause vision to become blurry.
In the early stages of some types of cataracts, glasses or contact lenses may help improve vision to some extent.
However, for most cataracts, surgery is usually is the only solution to improve vision.
What Is Done In Cataract Surgery?
In cataract surgery, the lens that has developed a cataract (which we will now only call ‘cataract’, for ease of understanding) is removed and is replaced by a clear artificial lens.
As mentioned above, the cataract is present inside a bag like structure that is suspended behind the iris by thread like attachments called the suspensory ligaments or zonules.
To remove the cataract, an opening is made in the bag that holds the lens. The cataract is then removed and a new artificial lens is placed in its place, inside the original bag.
The bag is cleaned before placing the artificial lens inside, so that it is clear at the end of surgery.
However, weeks, months to years after the surgery, the bag starts to become hazy. The haziness can be thought of as a kind of scar tissue that develops over time. This scar is called posterior capsular opacification or PCO.
Why Does Posterior Capsular Opacification (PCO) Develop?
No matter how well the bag is cleaned up at the time of surgery, a few microscopic lens cells always remain inside the bag. These lens cells can multiply over time and grow all over the bag.
The lens cells form scar tissue over the bag. This makes the bag cloudy and blocks light, resulting in blurry vision.
The blurriness from PCO increases over time as the scar tissue grows. If left untreated, it will cause more and more blurring of vision.
Remember that in cataract surgery, we make an opening in the front of the bag containing the cataractous lens, remove the cataract, and place a new lens in its place. So, the front of the new lens is not covered completely by the bag. The few lens cells remaining inside the bag and can only grow over the surface of the bag and not over the artificial lens. This is why PCO only forms behind the lens and not in front of the lens.
It is important to mention here PCO is present behind the lens, on the bag that holds the lens, while the lens itself remains clear.
Can Posterior Capsular Opacification (PCO) Be Prevented?
Modern surgical techniques have reduced the rates of PCO, but have not been able to eliminate it completely.
Some factors that may help reduce the chances of PCO include thorough cleaning of the bag at the time of surgery, and the use of specific artificial lens materials and designs.
Despite that, PCO can occur with the best surgical technique and materials, even in the hands of the best surgeon.
The younger the person is at the time of surgery, the greater the chance of developing PCO.
There that no precautions can be taken after surgery, to prevent or even reduce the chances of PCO developing.
The upside is that PCO can be easily treated with a simple, quick and effective laser procedure.
Symptoms of Posterior Capsular Opacification (PCO)
PCO causes symptoms similar to cataracts, which is why it is also known as ‘after cataract’. It is important to mention here that a cataract once removed, does not ever come back. PCO is only called ‘after cataract’ because it gives symptoms similar to cataracts.
Signs of PCO include:
- Blurring of vision
- Glare
- halos around lights
- poor vision in dim lighting
- double vision
How Is Posterior Capsular Opacification (PCO ) Diagnosed?
PCO can be seen inside your eye by your eye doctor, during a dilated eye examination at the slit lamp.
This exam is similar to the one you had before cataract surgery, with eye drops being placed in your eye to dilate the pupil and your eye being examined with the bright light at the slit lamp machine.
Treatment Of PCO – YAG Laser Capsulotomy
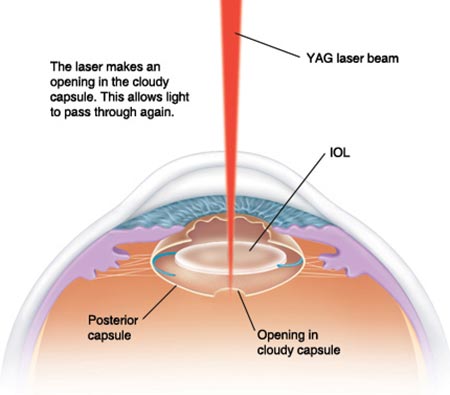
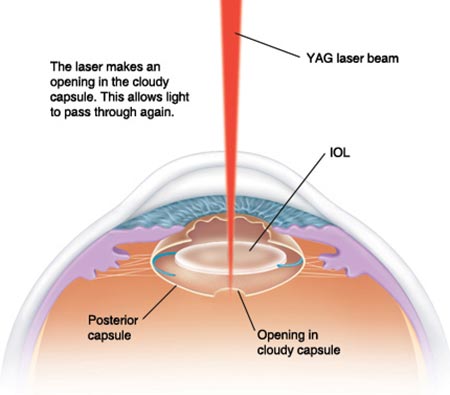
The good news about PCO is that it can easily be cleared up with a quick and painless, in-office laser procedure called YAG laser capsulotomy.
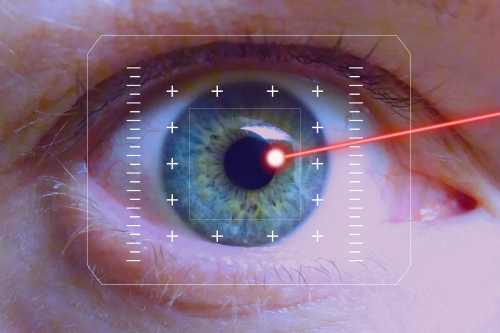
YAG laser is a special type of laser that creates an opening in the PCO formed at the back of your lens. It is named after the crystal – Yttrium Aluminium Garnet- that is used to produce the laser light. The laser light is focused so that it only targets the PCO and does not damage any other part of the eye. Once the PCO is removed by laser, the back of the lens clears up again and vision is restored.
Details of the Procedure
Before the procedure, eyedrops are placed in the eye, to numb the eye and dilate the pupil (colored part of the eye). It takes about 30-45 minutes for the dilating eye drops to take effect. Dilation of the pupil allows easier access to the PCO, which is present behind the lens.
You will be asked to sit at the YAG laser machine with your chin placed on the chin rest and forehead against the forehead rest. This laser machine looks exactly like the slit lamp machine the eye doctor normally uses to check your eyes.
Your head may be strapped gently against the fore head rest to avoid unnecessary head movements during the procedure.
A lens may or may not be placed on your eye, to aid the procedure. It will be held in position by the hand of the doctor. It might be slightly uncomfortable when the lens is placed on the eye, but once in place, you will not feel it. You will be asked to look at a target light.
The laser will then be used to create an opening in the PCO. The process will be painless and will take around 3-5 minutes. During the procedure you will hear beeping sounds and see flashes of light. After the procedure your eye pressure may be checked and you will be advised eye drops for home use for 1-2 weeks.
You might experience some light sensitivity and blurring after the procedure. This is due to the effect of the dilating drops, which lasts for around 6-8 hours.
Sometimes you may need another session if the PCO is too thick to be removed in one sitting or if the opening in the PCO was not made large enough to completely clear up your vision.
Once you have had this procedure, you will never need it again, as the scar tissue does not return.
Side Effects Of YAG Capsulotomy
A YAG capsulotomy for PCO has minimal risks, with serious complications being extremely rare.
Common minor side effects:
- If your eye was stabilized with a contact lens during treatment, you might experience slight discomfort after the procedure. However, this settles quickly.
- You might experience sensitivity to light and mild blurring of vision from the eye drops used to dilate the eye before the procedure. This will also settle in a few hours.
- A few floaters may develop in the eye after the procedure. These are from floating pieces of the scar tissue that was cleared up from behind your lens. Sometimes the YAG procedure may induce a posterior vitreous detachment (PVD) that can cause a large floater to appear in the eye. Floaters may or may not settle with time.
- In some individuals, the pressure inside the eye may rise after laser treatment for PCO, especially if they have pre-existing conditions like glaucoma. If you are at a higher risk of developing increased pressure in the eye, your doctor will monitor your eye pressure post-treatment and may prescribe medication to reduce elevated pressure. Increased eye pressure causes pain, redness, light sensitivity or blurring of vision.
Rare side effects:
Macular edema:
Sometimes YAG laser can cause swelling at the back of the eye (macular edema). This can cause blurring of vision. Macular edema from YAG laser can usually be treated with eye drops and oral medications. Sometimes if these are not effective, medication might need to be injected into the eye or very rarely a surgery (vitrectomy) may be required.
Breaks in the retina:
Very rarely, the YAG laser capsulotomy can cause breaks in the retina, leading to a retinal detachment. Individuals with high myopia are at a higher risk. Signs that you may have developed a break in your retina include flashes in your vision and sudden increase in the number of floaters. A retinal break needs to be sealed with another type of laser to reduce the chance of it developing into a retinal detachment.
Retinal detachment:
If you develop a curtain like shadow in the side of your vision, you may have developed a retinal detachment. A retinal detachment requires surgery to the eye for its repair and the sooner it is treated, the better are the chances of recovering vision.
If you develop lots of little black floaters, flashing lights or a shadow like curtain in your vision after YAG laser capsulotomy, report them to your eye doctor immediately.
Damage to the lens:
inaccurate focusing of the laser can cause laser damage to the lens, affecting its clarity. This happens when the procedure is performed by an inexperienced person.
Recovery After YAG Capsulotomy
You should not drive after the procedure as you may experience light sensitivity and blurring after the procedure from the eye drops used to dilate your eyes before the procedure
There are no other precautions you need to take and you can resume your normal day to day activities right away.
You can get your eye wet, use your cell phone, watch television, read, exercise or play sports right after the procedure.
If you were using glasses after your cataract surgery, you will still need to use them to see clearly
Commonly Asked Questions
Can I get YAG done to both eyes at the same time?
If you have PCO in both eyes, you can get YAG treatment done to both eyes, one after the other in the same sitting, so there is no need to schedule a second procedure at a later date.
Is YAG laser capsulotomy painful?
No, the procedure is painless. Numbing drops are placed in the eye before treatment. If your eye is stabilized with a contact lens during treatment, you might experience slight discomfort, however this settles quickly.
When can I return to work?
The day after the procedure. This is only because the dilating drops used before the procedure will cause light sensitivity and blurring of vision for a few hours.
Are there any precautions after the procedure?
You should not drive after the procedure as you may experience light sensitivity and blurring after the procedure from the eye drops used to dilate your eyes before the procedure
There are no other precautions you need to take and you can resume your normal day to day activities right away.
You can get your eye wet, use your cell phone, watch television, read, exercise or play sports right after the procedure.
When is the follow up after the procedure?
Follow up is usually not required after YAG capsulotomy, but do not hesitate to contact your doctor if you still have blurry vision after 24 hours after the procedure
Can YAG capsulotomy clear my vision if I have not had cataract surgery?
No. YAG capsulotomy is used to remove PCO (Posterior Capsular Opacification). PCO is a complication of cataract surgery. If you have not had cataract surgery, then you cannot have PCO. So, YAG capsulotomy cannot be used to clear your vision.
Can I develop PCO (Posterior Capsule Opacification) if I have not had cataract surgery?
No. Posterior Capsule Opacification, only occurs as a side effect of cataract surgery. If you’ve never had cataract surgery, you cannot develop PCO.
Will My Glasses Prescription Change After YAG Capsulotomy?
No, your glasses prescription remains the same after the procedure.
Are there any other treatments for PCO?
No, YAG laser capsulotomy is the only treatment for PCO. Glasses do not help improve blurring of vision from PCO.
Occasionally, if the PCO is too thick to be removed with YAG laser, it might need to be removed with surgery. However, that will involve a greater risk of side effects as compared to YAG capsulotomy.
Can I get YAG laser capsulotomy if I have other eye diseases?
If you have pre existing swelling at the back of the eye from other causes like diabetic eye disease, macular degeneration or vein occlusion, the swelling should ideally be treated before YAG laser is done.
This is because YAG laser itself carries a small risk of causing swelling at the back of the eye.
If you have glaucoma, your eye pressure will need to be monitored after the procedure as YAG capsulotomy can cause a temporary increase of the pressure inside the eye. You might also ne prescribed additional eye drops for a few days after the procedure, to control the eye pressure.